Pain is not simply a signs and symptom, it is a driver of physiology, decision-making, and individual trust. If you service the cutting edge, you really feel that stress when an individual grips your forearm and asks, "Can you flatter this?" The system PUAEME008 Supply Pain Administration supports that minute to repeatable, risk-free practice. It turns concept into muscle mass memory to ensure that you can assess, deal with, and reassess with tranquil efficiency, also when the alarms have not faded and the scene is still loud.

I have instructed and used these skills in rescues, country facilities, sports sidelines, and here aged-care centers. What separates positive medical professionals from reluctant ones is much less about pharmacology trivia and even more about routines constructed under assistance: a structured discomfort evaluation, a clear plan, clean communication, and regimented tracking. This post unboxes exactly how PUAEME008 maps to real shifts and genuine people, and where each technique earns its place.
Where PUAEME008 suits the community of training
Within emergency situation care and pre-hospital paths, PUAEME008 Give Discomfort Administration rests after fundamental life assistance and prior to advanced pharmacology or vital treatment components. It is frequently bundled with oxygen treatment, basic respiratory tract administration, and trauma treatment. For nurses and physiotherapists, it links the void in between discipline-specific evaluation and time-sensitive symptom control that maintains people relocating via treatment safely.
If you are scanning options for a discomfort administration course, you will certainly discover many brief courses in pain management that concentrate on persistent structures or certain professions. PUAEME008 Supply Pain Management strings a needle. It emphasises acute, time-bound choices that can be made in area, office, and occasion settings where you might be the most certified person on site. It dovetails with discomfort administration training for registered nurses who need regular analgesia procedures and with discomfort management courses for physio therapists that must comprehend when movement-based methods are reasonable and when medicinal or inhaled choices are safer.
Providers align their evaluations to administrative medication routines and professional practice standards. That implies a paramedic exercising in a metropolitan service might have accessibility to methoxyflurane or intranasal fentanyl, while a remote health and wellness employee may depend on dental analgesics and splinting. The system's toughness remains in process self-control, not the brand names.
The makeup of a robust pain assessment
Thorough discomfort analysis buys you everything that adheres to: appropriate treatment, less unfavorable results, measurable progress, and clear handover. The most typical failing I see is leaping right to a drug without comprehending the pain's system or trajectory. You will certainly do even more excellent by investing two extra minutes on evaluation than by rushing a dose.
Start with place, start, radiation, and personality. A person with right reduced quadrant pain that started periumbilically and moved may require medical referral greater than another dosage of analgesia. Seriousness ranges serve, yet just when anchored to operate. If a farmer rates his back pain as eight out of ten yet can still pivot from supine to sit with minimal guarding, you have a various trouble than the young athlete who calls it 4 out of 10 while sweating, tachycardic, and not able to bear weight.
Look for red flags: chest pain with diaphoresis, extreme migraine with neurological adjustments, distressing deformity with pallor and loss of pulses, unrestrained blood loss, or brand-new focal weak point. No discomfort management certification replaces professional judgment regarding when analgesia is second to respiratory tract, breathing, and blood circulation. PUAEME008 repeats that message till it sticks.
I favor discomfort tools that expand with the person. Start with a mathematical scale, then add a useful measure that fits the injury. After splinting a distal distance fracture, ask the child whether they can now wiggle fingers without rips and whether the discomfort goes down 2 factors. For a rib fracture, ask if they can take a fuller breath without a catch. Practical review makes your handover richer than a solitary number.
Non-pharmacological interventions that matter
The most forgotten section of any kind of give pain management course is the one without syringes. Easy actions frequently provide the fastest relief. Splint long-bone fractures before medicines. Placement clients with renal colic where they can relocate and extend the flank. Offload stress points with towels and cushions. Loosen limited clothing and ensure heat. Take into consideration ice for severe sprains in the very first day and gentle warmth for muscle spasm.
Coaching breathing is not simply for stress and anxiety. Sluggish diaphragmatic breathing wets sympathetic tone in injury and stomach pain. I utilize a four-second inhale and six-second exhale rhythm, duplicated momentarily, after that reassess the face and shoulder tension. The decrease suffering often shocks both client and bystanders.
Distraction has more trustworthiness than many provide it. In pediatric burns, the distinction in between a howling child and a calmer one during dressing originates from a tablet computer with an animation and a clinician who narrates what they are performing in basic, straightforward language. That tranquil lowers catecholamines and makes your pharmacology more effective.
Pharmacological approaches within scope
PUAEME008, when provided by credible companies, lines up with neighborhood formularies and service methods. While the particular medications vary, the logic does not: select the ideal drug for the pain type and setting, begin at a risk-free dosage, reassess immediately, and regard contraindications.
Oral analgesics are workhorses. Paracetamol and nonsteroidal anti-inflammatory drugs lower discomfort from stress, sprains, dental concerns, and mild to moderate fractures. If your pain administration training includes weight-based application and renal danger screening, you will prevent common mistakes. I fulfill many medical professionals that underrate dental options. When offered early, in the right mix, and sustained by immobilisation, they usually cut in half the demand for escalation.
Inhaled analgesia like methoxyflurane is prominent in some regions for brief, procedure-related discomfort in adults. It is quickly, titratable, and functions well for splinting or moving a person with limb trauma. Respect the complete dose restrictions and bear in mind queasiness. A pre-brief aids: discuss that the patient manages the inhaler, that it works within a couple of breaths, and that they must indicate if they feel dizzy.
Intranasal opioids, where offered within extent, are a solid option for modest to extreme pain when intravenous gain access to is not possible or would certainly delay treatment. They radiate in youngster fractures, rib injuries, and severe burns. Adhere to service procedures strictly. My very own technique relies on small, incremental application with a clear ceiling and very early antiemetics when indicated.
Topical agents like anesthetics have a narrower duty in emergency situation pain administration however can be useful in wound care and small procedures when within extent. Again, the training course stresses matching the agent to the task as opposed to memorizing brand name names.
Safety internet: contraindications, tracking, and side effects
The minute you provide analgesia, you have the monitoring. That is not paperwork, it is part of the treatment. Excellent courses in pain management training show you to keep track of three things constantly: discomfort relief, physiological stability, and adverse effects. Relief without stability is not success. Stability without relief is also not success.
Opioid-related sedation can creep. The individual talking one minute can plunge the following, particularly if tired out, hypoxic, or dried out. You do not require elegant equipment to identify very early modifications. Watch breathing rhythm, speech cadence, eyelid tone. Maintain the client upright if secure and reassess at two-minute periods after each dose change.
NSAIDs are not benign in dehydration, kidney illness, or peptic abscess. If you operate in hot environments or with older grownups, ask about diuretics and antihypertensives before you reach for ibuprofen. Paracetamol's ceiling matters. Prevent stacked dosing from numerous sources. Individuals often take mix cold tablet computers that conceal added paracetamol.
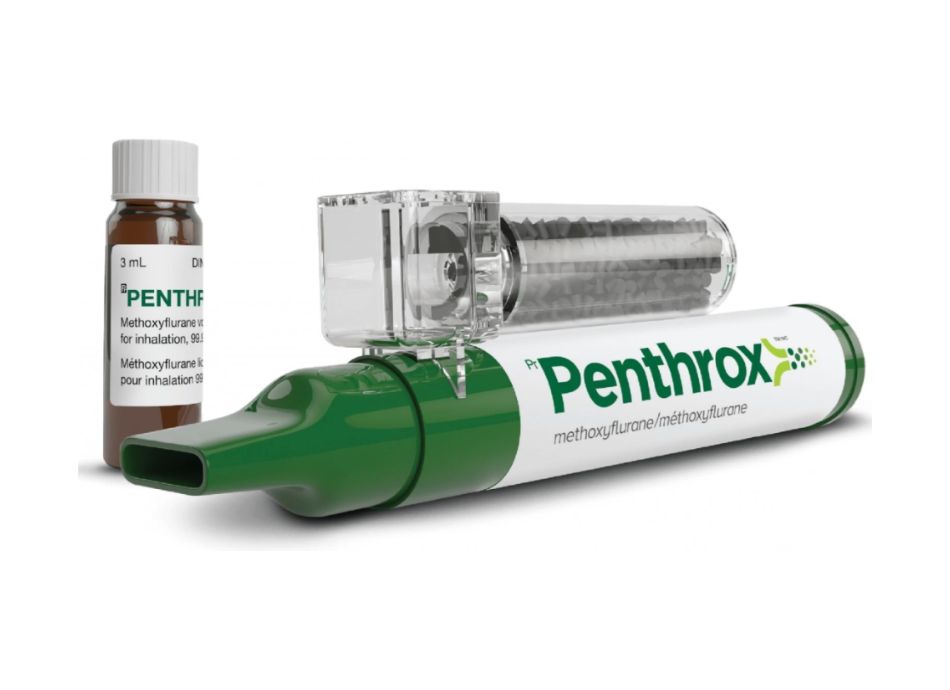
Methoxyflurane's complete dosage limits and carrier exposure limits are well publicised. Adhere to them. Pre-oxygenate hypoxic people before you begin. Fasting is not a prerequisite for inhaled or oral analgesia in the field, yet strategy ahead if sedation or transfer could be necessary.
Documentation that earns trust fund at handover
Good documents is not a formality, it is a handover of responsibility. A clear record of discomfort beginning, qualities, assessment ratings, useful effect, interventions, and the timeline of doses assists the next medical professional stay clear of replication and complications. When I give a handover after a road crash, I consist of three timestamps: when I first evaluated discomfort, when I delivered the crucial intervention, and when the pain enhanced by at least two factors. That pattern, repeated throughout a solution, boosts quality of care.
If your company makes use of electronic platforms, enter your monitorings in actual time if risk-free. Otherwise, jot shorthand on your handwear cover or tape and transcribe later on. Make every number purposeful. "Discomfort 9/10 to 5/10 after splint and breathed in analgesia, client currently able to move onto inside story with mentoring" says more than "pain enhanced."
The human aspect: communication under stress
Pain makes individuals frightened, and fear enhances pain. A stable voice that describes what you are doing decreases both. Stay clear of the lure to overpromise. I tell people specifically what the treatment could attain: "This need to puaeme008 compliance requirements soothe so you can take a breath and relocate. It will certainly not erase the discomfort completely, but you will certainly be more secure and much more comfy while we treat the reason." Underpromise, after that supply noticeable improvement.
Family members can be allies or amplifiers of distress. Provide a role: hold a hand, hint the breathing, fetch a covering. It channels power far from panic and toward treatment. For children, offer selections that do not endanger safety. "Do you want the blue pillow or the white one under your arm?" Control over small points makes analgesia extra effective.
Where PUAEME008 satisfies details settings
In commercial websites, emergency discomfort monitoring usually starts with entrapment or crush injuries. The priorities shift to bleeding control, splinting, and early analgesia to blunt the catecholamine surge. Thermal exposure, sound, and restricted room complicate both assessment and inhaled choices. The training emphasises scene safety and security, rapid extrication methods, and interaction in high-noise environments. Small techniques matter, like pre-explaining to an individual that the inhaler odor is strong and regular, so they are not alarmed in a dark space.
In sports events, the difficulty is distinguishing joint sprain from fracture swiftly and deciding who can walk and who must be immobilised. Physios with discomfort monitoring programs for physiotherapists frequently excel right here since they mix packing tests with analgesia and know when to intensify. The unit's framework assists non-physio medical professionals prevent tunnel vision on discomfort ratings and think about joint stability and neurovascular standing first.
In aged care, polypharmacy and frailty control the danger profile. NSAIDs may be off the table. Opioids call for reduced starting doses and closer respiratory system tracking. Non-pharmacological measures come to be main. Padding bony importances, slow-moving transfers, and hydration can alter the pain landscape without a solitary tablet computer. Registered nurses that full pain management training for nurses report less transfer delays and even more foreseeable reactions when they adopt a typical assessment and titration sequence.
Scenario walk-throughs that mirror genuine shifts
A country rollover, single owner, mid-30s. Mindful, groaning, forearm defect, and best chest inflammation. On method, you determine that analgesia will assist you analyze the breast correctly and use a splint. You warm the individual, apply high-flow oxygen, and train sluggish exhalations while your companion subjects and palpates gently. With important signs stable, you start breathed in analgesia within extent, always staying below dose caps and maintaining antiemetic prepared. You splint the lower arm, pad the ulnar head, and secure fingers. Discomfort drops from 8 to 5. Now the individual can take deeper breaths, and you can check out for crepitus. You record times, dosages, functional change, and you hand over with self-confidence at the obtaining facility.
A teenager with a severe ankle injury at a netball event. No open injuries, swelling and defect around the lateral malleolus, neurovascular status undamaged. You elevate and use a vacuum cleaner splint before any type of medications. Paracetamol and an NSAID are provided orally after checking for allergic reactions and last dosage. Taking a breath mentoring and diversion with a colleague's assistance decrease anxiousness. Discomfort drops from 7 to four within 15 mins, enough to enable a mild transfer to the vehicle for radiology. The record consists of a clear strategy and red flags that would set off ambulance transfer.
An older adult with shoulder pain after a bathroom slip. They look pale and protect their side. Important signs show mild tachycardia. You believe rib cracks or a humeral neck injury. You pad the axilla, placement for comfort, and prevent existing level. Oral analgesics are begun meticulously given age and comorbidities. You choose against inhaled analgesia due to nausea or vomiting and take into consideration intranasal alternatives if within scope, with incremental doses and sluggish review. The client can now breathe much deeper and endure transfer. You call in advance to the emergency situation division with a crisp recap and explicit dosage totals.
What a top quality pain monitoring program looks like
Courses vary extremely. The best pain management courses invest much less time lecturing regarding receptor subtypes and more time on practical scenarios with imperfect details. If you are comparing pain monitoring training programs, seek three features.
- Live situation exercise with timed reviews and developing client conditions. You desire representatives under moderate stress, not simply PowerPoint slides. Clear placement to neighborhood protocols and range, including drug schedule, dose limits, and documentation requirements. Generic web content ages fast. Assessment that consists of communication and paperwork, not just medicine calculations. Actual care is greater than math.
When a program promotes a discomfort monitoring certification, ask about revival assumptions and whether the service provider audits grads' documents quality. A pain management certificate training course without any continuous top quality loop typically discolors right into trivia after six months. For medical professionals in controlled environments, a pain management accreditation program need to incorporate with existing medical governance, event coverage, and medicine handling standards.
The trade-offs you only learn on the road
Titration speed is a consistent balancing act. The lure to front-load analgesia in a client that appears calm commonly backfires during motion when hidden instability causes an abrupt pain spike and nausea or vomiting. Incremental application with clear ceilings preserves alternatives. On the other hand, underdosing a patient with a femoral shaft fracture prolongs suffering and makes every succeeding action harder. Experience shows you to review micro-signs: the method the jaw collections, the micro-guarding on palpation, the breath hold just before a movement. PUAEME008 provides you the framework to pair with those instincts.
Another compromise rests in between procedure timing and analgesia start. It can be suitable to begin splinting as the breathed in agent works as opposed to awaiting a total decrease in pain. The key is pre-briefing the person and coordinating movements. Countdowns, foreseeable touch, and a clear quit signal make half the difference.
Finally, scene rhythm matters. A disorderly scene with multiple onlookers frequently pressures you right into hurrying. The antidote is a 20-second reset. Inform your group aloud: "Evaluation full. Strategy: splint initially, breathed in analgesia, then relocate." That brief affirmation aligns activities and calms the patient that hears that you have a plan.
For nurses and physio therapists considering official training
Nurses asking whether to buy an offer discomfort management program need to weigh 2 benefits beyond analgesic ability. Initially, uniformity across changes. When every nurse makes use of the very same evaluation and titration pattern, individuals relocate with wards and divisions with less jolts in their pain control. Second, documentation high quality that sustains audit, research study, and high quality enhancement. Many services currently track door-to-analgesia times, reassessment intervals, and nausea or vomiting prices. Educating products the habits that enhance those numbers.
Physiotherapists often think twice, anxious that medicinal content rests outside their everyday work. In method, the training course enhances your safeguard. You will acknowledge when a movement-based method needs time out, when reference is urgent, and just how to connect concerning analgesia options without violating scope. If your practice includes occasion protection or sports trauma, the advantages are instant. Pain monitoring programs for physiotherapists that consist of splinting, taping complements, and return-to-play decision frameworks tend to deliver the very best transfer to field settings.
Building proficiency after the certificate
A single certificate training course does not make expertise. You construct that with deliberate practice. After completing PUAEME008 Give Discomfort Management, set a three-month strategy. Pick two common scenarios in your setting, possibly wrist fractures and renal colic. Track your very first analysis time, time to first analgesia, reassessment period, and patient-reported practical change. Testimonial a handful of cases monthly with an associate. The pattern acknowledgment you acquire from reflective method beats random repetition.
Seek feedback from individuals as well. A solitary question jobs: "Did you feel your pain was taken seriously and dealt with quickly?" Collect those feedbacks. When ball game dips, check out. You will commonly find system problems like postponed accessibility to medications or incomplete handovers that training can remedy.
What not to ignore before you enrol
Check that the training service provider acknowledges regional laws. In some regions, methoxyflurane or intranasal opioids might not be authorised outside details solutions. If your role limits you to oral choices, make certain the training course still shows innovative non-pharmacological approaches and scenario decision-making as opposed to spending a lot of the day on restricted drugs.
Confirm that the pain management certification consists of analysis of proficiency, not simply participation. You want situations with trainers who watch your micro-decisions and push back when you drift. Ask whether the certificate program suffering monitoring consists of pediatric and senior citizen subtleties. Those 2 populations expose weak structures quickly.
Finally, try to find integration with your wider continuing expert growth. Programs that connect to an abilities profile, supervisor sign-off, and regular refreshers deliver even more worth than stand-alone certificates.
A short guidebook you can carry in your head
- Assess cause and danger before you go after numbers. Red flags surpass discomfort scores. Use non-pharmacological procedures early. Splint, setting, warm, instructor breathing. Start with suitable, locally accepted analgesia, titrate in tiny steps, and display closely. Reassess feature, not just numbers. Then record clearly and hand over with timestamps. Communicate assumptions honestly. Calm words enhance every treatment you deliver.
The real-world payoff
When discomfort management ends up being a consistent, practiced regular, you quit firefighting and start leading the scene. Clients pick up that and loosen up right into your treatment. Transfers run smoother. Less people vomit in ambulances. Less older grownups end up being delirious from unnecessary polypharmacy. Associates count on your handover notes. The little effectiveness pile: 5 minutes conserved right here, a difficulty stayed clear of there, a much better experience logged in a problem system that usually just finds out about the misses.
PUAEME008 Give Pain Administration is not attractive, however it is the scaffolding that sustains virtually every other clinical ability you utilize under stress and anxiety. If you are picking among pain administration programs, choose one that drills process, sharpens judgment, and respects the facts of your range and setting. The certificate on your wall will be the least important outcome. The new calm in your technique will certainly be one of the most visible one.
